 This week we spoke with Associate Professor Chris Judkins, an Interventional Cardiologist working in Fiona Stanley Hospital. He consults privately in Murdoch, Katanning, Palmyra, Midland and Narrogin. Dr Judkins provides a comprehensive cardiology service including telehealth cardiology.
This week we spoke with Associate Professor Chris Judkins, an Interventional Cardiologist working in Fiona Stanley Hospital. He consults privately in Murdoch, Katanning, Palmyra, Midland and Narrogin. Dr Judkins provides a comprehensive cardiology service including telehealth cardiology.
He has submitted a very useful summary of a common cardiology presentation in GP. Feel free to leave any comments or queries for Dr Judkins to respond to.
View Profile in GPHQ directory
Advice: 0414 468 332 Consultations: 08 9366 1899
Chest pain presentation in General Practice is common. Around 15% of patients will present to their GP as the initial point of contact. The causes for chest pain are many and varied.
What is the safest and most accurate way to investigate suspected cardiac chest pain?
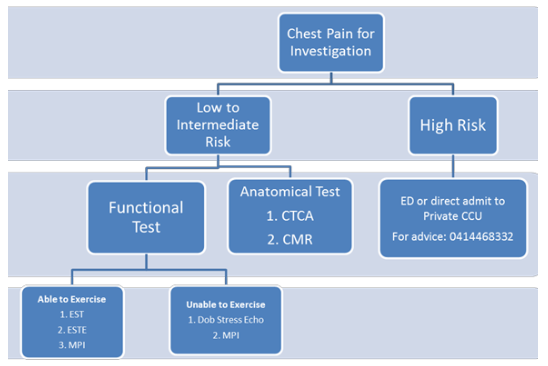
- High-risk patients requiring monitoring and troponin assays should in most cases be sent through to an Emergency Department or direct admitted to a CCU privately.
- If the patient is pain-free for >12 hours and not considered “high risk” they may be investigated in the outpatient/GP setting.
What is the best non-invasive test for patients not requiring ED review?
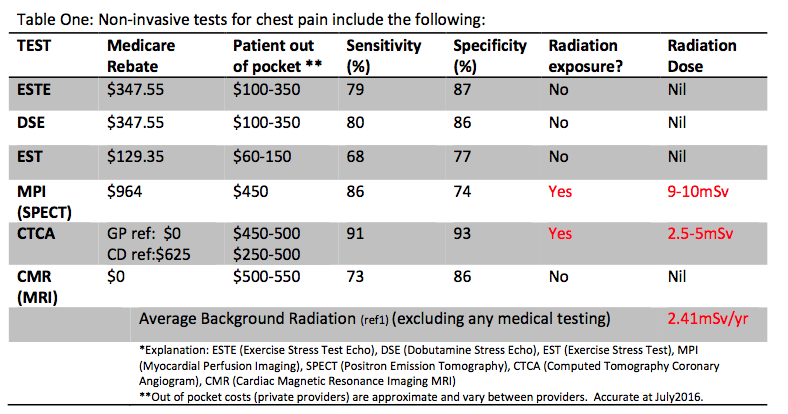
The “best test” depends on the question being asked and the information required. It also takes into account radiation exposure, cost and availability. These will differ depending on the patient and locality. Tests can be divided into functional *(ESTE, DSE, EST, MPI and CMR) and anatomical (CTCA, CMR).
The choice of test will depend on the patient’s symptoms, co-morbidities, ability to exercise and clinical concern. The first question to ask is “If I get a normal noninvasive test will I be comfortable to believe the result?” If the answer is no then invasive coronary angiography may be the preferred strategy. If the answer is yes (as it will be for the majority of patients), consider the algorithm below to guide decision making.
Important Comments on testing
- Exercise testing is preferred over pharmacological testing (e.g. Dobutamine) where possible.
- For patients without recent heart attack or moderate-severe heart failure, beta-blockers or other rate control agents should be withheld 24 hours prior to stress testing.
- For CTCA, rate control agents should be continued as a low heart rate is required for imaging.
- Where coronary angiography is to be performed, there is compelling data to support radial artery access by high volume operators with less bleeding and bruising complications.
- Referral to an interventional cardiologist for coronary angiography will allow treatment to be combined with diagnosis, decreasing inconvenience and repeat procedures for the patient.
Radiation Considerations:
There is enormous variation in radiation exposure between the tests. Exercise Stress Test Echo has the lowest risk with no radiation exposure. Table 1 above lists the radiation exposure for each test. As a guide, a CTCA is between 1-2 years of background radiation and an MPI is 3-4 years of background radiation.
Cost Considerations:
All testing has a cost in terms of equipment and staffing. The total cost is the combined out of pocket cost and the taxpayer funded cost again with significant difference between tests. MPI has the highest total cost. ESTE, DSE and EST have the lowest out of pocket cost for patients.
Availability Considerations
ESTE, DSE, EST, CTCA and MPI are readily available. Publically available ESTE, DSE and EST are not easily available however WA Cardiology caters for public and private patients and provides competitive pricing.
Stress Testing
Exercise Stress Test Echo (ESTE)
ESTE is an EST with the additional benefit of echocardiographic imaging. This is an ideal test for most patients who are able to exercise with excellent sensitivity and specificity (equal to MPI), and allows for assessment of valvular and left ventricular function. There is no radiation exposure (unlike MPI) and tests are easily available and cheaper than MPI and CTCA. Image quality may be compromised in obese patients.
Dobutamine Stress Echo (DSE)
DSE is similar to an ESTE with ECG and Echocardiographic assessment but is ideal for patients who can’t exercise on a treadmill or bike. The DSE provides the same information as an ESTE and again without radiation exposure.
Exercise Stress Test (EST)
ESTs have a lower sensitivity and specificity than the other testing modalities, however is widely available. False positives are more common, particularly in middle aged females. Consider avoiding EST in the middle aged female population. Patients with abnormal ECG such as LBBB are not suitable for EST. Consider an ESTE in these populations.
Myocardial Perfusion Imaging (SPECT, PET)
MPI (SPECT or PET) identifies areas of myocardium with decreased blood flow. The test usually requires 2 appointments over two days. SPECT has the highest radiation exposure of any of the non-invasive tests (3-4 years of background radiation) while PET is similar to CTCA. Generally MPI is more expensive than EST or DSE/ESTE. MPI may be false negative if triple vessel disease is present. In morbidly obese patients MPI may provide better imaging quality than echo based tests and provides a good assessment of LV function.
Computed Tomography Coronary Angiogram (CTCA)
CTCA is a noninvasive anatomic test and is excellent as a rule out test in low to intermediate risk patients. It’s less useful where known coronary artery disease exists, or with extensive arterial calcification (eg diabetics). While the radiation doses have come down in recent years this remains operator dependent, equivalent to 1-2 years of background radiation per test. There is no GP referred Medicare rebate and the test remains moderately expensive. CTCA has the additional benefit of Calcium scoring to risk prognosticate (only useful over the age 50).
It’s important to note that CTCA (anatomic imaging) and a Calcium score measure two different things. CTCA provides information on current flow limiting lesions and overall plaque burden. A Calcium score provides a measure of future risk of a cardiovascular event and can guide aggressiveness of risk factor management.
Cardiac MRI (CMR)
Cardiac MRI is more difficult to access and is often used where questions of muscle viability are required prior to planning revascularization. It is also useful to differentiate between myocarditis and ischemia. This test is usually reserved for specialist referral. While CMR has no radiation dose if radioisotopes are used (eg gadolinium) then there is a radiation exposure.
Coronary Angiography
Coronary Angiography (CA) remains the gold standard investigation. CA is more invasive with radiation exposure but again there are decreasing doses with modern equipment (measured in mGy/cm2). There are minimal bruising and bleeding risks when performed radially (via wrist). The advantage is that stenting (treatment) can be performed at the same time when appropriate if the operator is trained in interventional cardiology. CA is an excellent test where a high suspicion for functionally significant coronary artery disease exists. In addition if a narrowing is of borderline significance the use of fractional flow reserve (FFR) has been shown to improve patient outcomes by identifying those patients who will benefit most from stenting. This is performed at the time of coronary angiography. Dr Judkins is a gap-free provider so there is no out of pocket expense for private patients requiring coronary angiography or coronary intervention.
Ref 1: United Nations Scientific Committee on the Effects of Atomic Radiation (2008). Sources and effects of ionizing radiation. New York: United Nations (published 2010). p. 4. ISBN 978-92-1-142274-0. Retrieved 9 November 2012

