Dr Rob Nairn is a Musculoskeletal Radiologist with Perth Radiological Clinic.
Dr Rob Nairn is a Musculoskeletal Radiologist with Perth Radiological Clinic.
He entered the Western Australian Radiology training programme in 2006 and in 2010 he completed his radiological studies. He then commenced a year long musculoskeletal fellowship training position at The Ottawa Hospital/University of Ottawa, Canada. He completed his fellowship training in July 2011 and returned to Western Australia joining Perth Radiological Clinic in August 2011. He became a Partner in 2015.
He completed his fellowship training in July 2011 and returned to Western Australia joining Perth Radiological Clinic in August 2011. He became a Partner in 2015.
MRI Knee – Key Points
|
What is the MBS item description for knee MRI?
Acute knee trauma in a patient 16 or older with:
- Inability to extend the knee suggesting the possibility of acute meniscal tear
- Clinical findings suggestive of anterior cruciate ligament tear
Acute knee pain following an injury is a common clinical problem. Xrays are used to exclude fractures and are very useful in the acute period. MRI can safely and accurately diagnosis internal knee derangement, obviating the need for diagnostic arthroscopy if a “wait-and-see” management is adopted. This talk will briefly discuss two important elements of knee MRI, namely ACL tears and meniscal tears.
 PART 1: Anterior Cruciate Ligament tears
PART 1: Anterior Cruciate Ligament tears
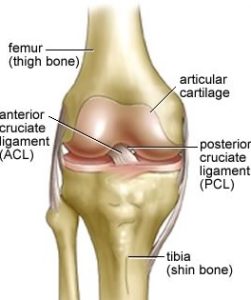
The anterior cruciate ligament is a key stabilizer of the, acting to prevent anterior translation of the tibia on the femur. The ACL runs anteroinferiorally form the posterior intercondylar region of the distal femur, to the anterior aspect of the tibial eminence. The ligament is composed of collagen fibres coalesced into two discrete “bundles”, the anteromedial and posterolateral. The ACL is covered by synovium anteriorly and laterally but is actually outside the synovial membrane, analogous to the retroperitoneal portion of the duodenum. The ACL usually tears/fails in adults at its substance, or at its enthesis (insertions) in kids

Can plain films help with ACL?
- On Xray in the acute setting, absence of an effusion effectively excludes the possibility of an acute ACL injury
- Several subtle Xray findings can suggest ACL tearing, outside the scope of this discussion
- The role of Xrays in the acutely traumatized knee remains assessing for fractures and effusion
What are the associated findings of ACL tears?
Associated findings of an ACL tear are commonly seen on MRI, and injuries to other important structures are also commonly seen. These include:
- Vertical tears of either or both menisci
- Tibiofemoral bone bruises/subchondral fractures
- Joint effusion (always in the acute setting, but may resolve in a few weeks)
Indirect evidence implying ACL insufficiencyIndirect evidence implying ACL insufficiency
- Anterior translation of the tibia on the femur – the MRI equivalent of Lachman’s test positivity
- Buckling of the PCL or patellar tendon – both structures should normally appear taut
- “straightening” of the LCL
 Loading...
Loading...
 Loading...
Loading...
PART 2: Meniscal Tears
- Meniscal tears are very common in the acutely traumatized knee
- MRI is the modality of choice for investigating meniscal derangement noninvasively
- GP rebates for acute meniscal tears now means the role of CT arthrography is much reduced, and in general MRI of the knee should supplant CT arthrography for virtually all knee clinical scenarios. CT arthrography is more invasive, requiring direct injection of contrast into the joint
- Two are present, medial and lateral. Composed of fibrocartilage
- The peripheral 1/3 of menisci has blood supply, so tears that are purely peripheral are candidates for meniscal repair rather than resection/partial meniscectomy. Tears that involve the central 2/3 are generally treated with partial meniscectomy
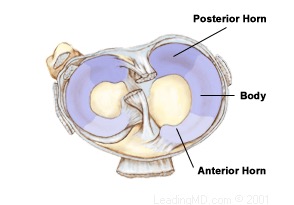
- Radiologists divide both menisci into an anterior horn, body, posterior horn and anterior/posterior root attachments (to the tibial eminence)
Meniscal Anatomy MRI
Normal menisci on MRI should:
- Be of uniformly low signal (“black”) on all pulse sequences
- Have normal morphology
- No displaced fragments
On the sagittal sequences, look for the “bow-tie” appearance of the anterior and posterior horns. On the coronal sequences, look for the normal triangular shape of the meniscal body, converging to the sharply defined meniscal apex

Meniscal Tears
MRI definition of meniscal tearing is very simple:
- Abnormal morphology, and/or
- Linear high signal on 2+ slices contacting the articular surface of the meniscus
Radiologists often describe tears based on their orientation. Two major orientations are vertical and horizontal (oblique means not quite either). Tears are commonly complex (vertical and horizontal components)
Stability: by definition, all displaced tears are unstable, but many meniscal tears are potentially unstable
Common Meniscal Tears
Remember, all tears are either vertical or horizontal, or a combination of vertical and horizontal.
- Bucket-handle: vertical tears with displacement of meniscal tissue towards the intercondylar region
- Radial: orientated along the short axis of the meniscus, from its periphery to the apex/free margin
- Flap: unstable oblique undersurface tears, usually of medial meniscus posterior horn, commonly have displaced meniscal fragments and or subarticular stress responses or even insufficiency fractures
- Peripheral vertical tears usually seen in relation to ACL tears, are potentially repairable if contained to the vascularised periphery of the meniscus.

Ancillary signs of a meniscal tear
- Knee effusion – may or may not be present
- Displaced meniscus fragment – by definition, must have a meniscal tear
- Parameniscal cyst – fluid collection abutting the meniscus periphery; implies tearing is present
- Subarticular bone marrow oedema – due to altered biomechanics following meniscal tearing. May progress to a subchondral insufficiency fracture
Subchondral insufficiency fractures were previously called Spontaneous Osteonecrosis of the Knee (“SONK”), a term radiologists try to avoid using (as it’s not spontaneous, and the major aetiology is not osteonecrosis)

Menisci in the Elderly
- Tears in the middle aged and elderly are relatively common, and increase in incidence as we age
- Meniscal tears may not be clinically relevant in the elderly, particularly if the knee is arthritic
- “degenerative” meniscal tears in arthritic knees are very common
- Correlation of your patient’s history and clinical signs and symptoms is even more important when interpreting MRI reports than in the young
ie, the role of history and examination is even more important in interpreting MSK imaging in the elderly!
We would like to thank Dr Nairn and Perth Radiological Clinic (PRC) for taking the time to put together this very useful summary article. PRC offers short waiting lists for MRI, urgent same day reports on request and has 11 MRIs in the Perth Metro area. All MRIs are reported by radiologists with specific MRI training. They have numerous fellowship-trained subspecialty MSK MRI reporters.
Users are welcome to leave comments below.