This week we spoke with Professor John Olynyk. Professor Olynyk is the Head of Gastroenterology at Fiona Stanley and Fremantle Hospitals Group, Director Research Development South Metropolitan Health Service WA and Professor of Translational Medicine at Edith Cowan University.
This week we spoke with Professor John Olynyk. Professor Olynyk is the Head of Gastroenterology at Fiona Stanley and Fremantle Hospitals Group, Director Research Development South Metropolitan Health Service WA and Professor of Translational Medicine at Edith Cowan University.
He is a medical advisor to the Haemochromatosis Society of Australia and a consultant for the Australian Red Cross Blood Service. He has established internationally recognized research programs in Hereditary Haemochromatosis and other iron disorders, chronic liver injury and adolescent non-alcoholic fatty liver disease.
Professor Olynyk has submitted a very useful summary on the Management of Haemochromatosis in Primary Care.
View Profile in GPHQ directory
-When should GPs suspect Hereditary Haemochromatosis (HH)?
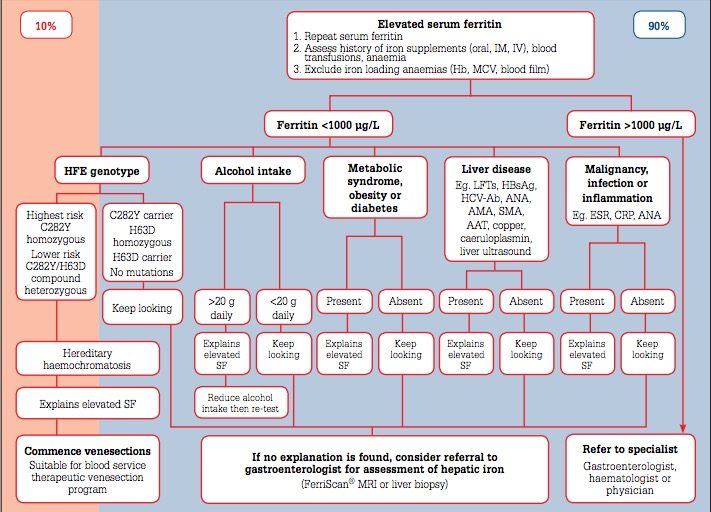
The clinical features and symptoms that could be suggestive of HH include lethargy, fatigue, arthritis (Symmetrical and usually of hands, hips or other large peripheral joints), hypogonadism. Signs – pigmentation, arthritis, liver disease. Family history of HH. Iron results – ferritin elevated above reference range and almost always with elevated transferrin saturation as well (see algorithm below)
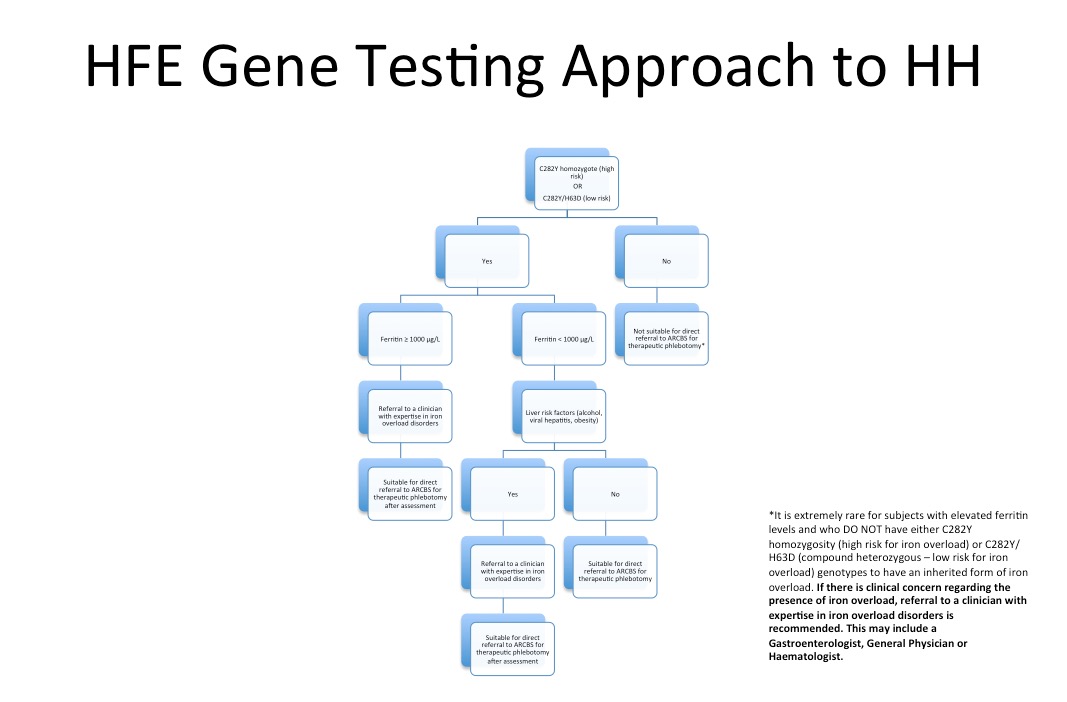
-Can you tell us about the interpretation of genetic testing?
- High risk for iron overload – C282Y homozygosity. The risk a patient will develop significant iron overload by 60 years is up to 40% of men and 10% of women with this genotype. i.e. the majority won’t.
- Low risk – all other genotypic combinations
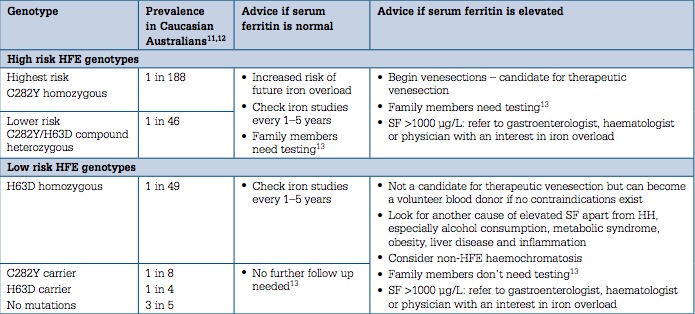
-When advice would you give on management based on HFE genotype and serum ferritin?
The table below summarises this best.
-What is the ferritin target when performing venesections?
The target ferritin is low normal range, approximately 50-100 ug/L. The following is a useful schedule to follow.
| Iron unloading phase, target serum ferritin ~50 µg/L |
| Weekly venesection of ~7 mL/kg (maximum 550 mL) whole blood. Ensure pre-venesection haemoglobin >120 g/L
Monitor Hb and serum ferritin:
It may take many months or even years to unload excess iron. Oral vitamin B12 and folate supplements support erythropoiesis during frequent venesections |
| Lifelong maintenance phase, target SF ~50–100 µg/L |
| Venesections to maintain serum ferritin ~50–100 µg/L s
Highly variable between individuals, often in the range 2–6 venesections per year. Monitor serum ferritin at least every 12 months |
-What are the eligibility criteria for Australian Red Cross Blood Service Therapeutic Venesection program?
Evidence of hereditary haemochromatosis:
- C282Y homozygosity
- C282Y/H63D compound heterozygosity
Clinical iron overload supported by FerriScan® MRI or liver biopsy
Polycythaemia Rubra Vera
Porphyria cutanea tarda
-How often do you check FBC and ferritin in primary care?
Each phlebotomy session will reduce ferritin by about 40-50 ug/L so this is how often I monitor their ferritin and Hb:
- During acute treatment phase (weekly phlebotomy) – monthly
- During 2 weekly therapy – 2 monthly
- During maintenance – 6 monthly or annual ferritin
Other key messages:
|
We would like to thank Professor Olynyk for taking the time to put together this very useful summary article. Users are welcome to leave comments below.